
Seattle Children’s Cardiac Beat
Winter 2023

Dear Colleagues,
Welcome to the inaugural edition of Seattle Children’s Cardiac Beat. Our Heart Center team is excited to present you with news and information about the latest diagnostic, therapeutic and research advances in cardiovascular diseases and cardiac surgery at Seattle Children’s.
This first issue introduces you to the new, state-of-the-art cardiac procedural suites on Seattle Children’s Hospital campus, a groundbreaking study about an adjustable heart stent for children with coarctation of the aorta, the latest thinking on fetal echocardiograms, and the results of a study designed to decrease ventilator-associated tracheitis (VAT) in the Cardiac Intensive Care Unit.
We welcome your feedback about the types of news or articles you find most valuable to your practice. Please feel free to email us with suggestions at janna.hendrickson@seattlechildrens.org or contact us to find out more about Seattle Children’s Heart Center, to refer a patient or to schedule your patient for a fetal cardiac consultation.
Thank you for your interest in our Center,
Mark B, Lewin, MD, Division Chief, Cardiology; Co-Director, Heart Center; Medical Director, Fetal Care and Treatment Center
Michael McMullan, MD, Division Chief, Congenital Cardiac Surgery; Co-Director, Heart Center Surgical Director, Cardiac Transplantation
New State-of-the-Art Facility Doubles Seattle Children’s Cardiac Surgical Capacity and Exceeds Safety Standards

Dr. Brian Morray, director of Seattle Children’s Cardiac Catheterization Laboratories, confers with a cardiac patient in one of Forest B’s new spaces.
Seattle Children’s Heart Center has a new, state-of-the-art home in Forest B, the 310,000-square-foot addition to Seattle Children’s hospital campus specifically designed for transformative, patient-centered care.
The Heart Center occupies nearly 30,000 square feet on the sixth floor of the new building. The dedicated space doubles the number of operating rooms devoted to cardiac patients and co-locates the cardiac induction rooms, operating rooms (OR), catheterization labs, post-anesthesia care unit (PACU) recovery rooms and cardiac ICU into what is known as the Heart Center Suites. Although the cardiac ICU is technically located in Forest A, it is separated from the ORs by a three-foot walkway.
This co-location of services greatly reduces patient transport time and facilitates those times when a patient needs to go quickly from the catheterization laboratory to surgery, or from surgery to a cath lab.
Dr. Brian Morray, director of Seattle Children’s Cardiac Catheterization Laboratories, said “with the new facilities, it's now just a matter of literally moving the child to the room adjacent rather than down the hall or going to a different building. In co-locating those services, I think we will really enhance patient outcomes and improve patient safety.”
The new co-located space also enhances the relationship between cardiology and cardiac surgery. According to Morray, “it enables our skillset to enhance surgical outcomes and the surgical skillset can enhance our outcomes in the cath labs. And that's a very important and unique feature of this new space that isn’t found in many other pediatric facilities.”
A focus on patient safety
Seattle Children’s Heart Center is one of the top ranked programs of its kind in the United States. The Heart Center team includes more than 70 board-certified pediatric surgeons and cardiologists who treat children from before birth through young adulthood with all kinds of heart defects – from the most common to the most complex and rare. Our team performs more complex pediatric heart procedures than any other provider in the region and is rigorously focused on safety and achieves some of the top patient outcomes in the nation.

One of the Heart Center’s new state-of-the-art operating rooms.
To ensure a safe environment in the new Forest B Heart Suites, the air supply for the ORs and catheterization labs is filtered through HEPA (99.97%) filters twice, once at the air handling unit prior to the air entering the duct system and a second time in the ceiling of each room just before the air enters the space. Washington State code calls for one level of MERV 14 (90 to 95%) filtration in operating room environments either at the air handling unit or at the room.
Dr. Michael McMullan is the division chief of Congenital Cardiac Surgery and co-director of the Heart Center at Seattle Children’s. He says, “this new building exceeds all of the normal standards to make sure our patients are safe. The fact that the ventilation goes so far beyond the standard is just one more example of how we've gone all out to build the safest and most technologically advanced facility possible.”
Patient safety is also addressed in the new catheterization labs. Both labs are equipped with the most up to date Siemens fluoroscopy equipment, which deliver lower doses of radiation to patients. According to Morray, “Not only are the lower radiation doses important for our patients’ long-term health, but the new equipment gives us sharper X-ray images, which allows us to do more complicated procedures and work with smaller children.”
Continue Reading about the New State-of-the-Art Cardiac Facility
Adjustable Pediatric Heart Stent Moves to Pivotal Trial
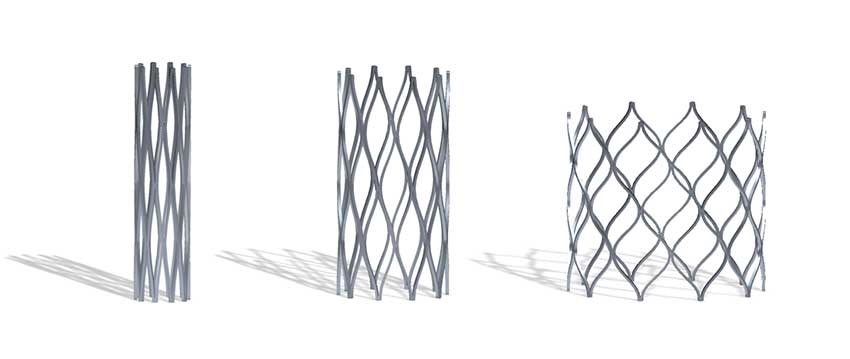 The Renata Minima Stent can be gradually expanded up to adult size over the course of the child’s lifetime.
The Renata Minima Stent can be gradually expanded up to adult size over the course of the child’s lifetime.
Infants and children with congenital heart disease are one step closer to a lifelong solution, thanks in part to Seattle Children’s Heart Center team.
In spring, 2022, Seattle Children’s was one of only four pediatric hospitals in the nation to participate in an early feasibility study of a new minimally invasive cardiac stent developed to treat narrowing of the pulmonary arteries or the aorta. Designed to expand as younger patients grow, the Renata Minima Stent holds the promise of reducing the need for repeated risky and expensive open-heart surgeries to replace stents that have become too small.
According to Dr. Brian Morray, Director of Cardiac Catheterization Labs at Seattle Children’s, “there’s a huge need for this technology. There are currently no FDA approved stents for use in pediatrics. “
Pediatric stents present challenges not found in adults–namely that adults will not outgrow their stents. With young children, and infants in particular, stents become ineffective as their arteries grow, requiring them to be redilated or replaced at multiple points during their lives.
“Developing a stent that’s small enough for an infant but can accommodate for growth is an engineering challenge that most companies have not been willing to take on,” said Morray.
“The fact that this stent is designed specifically for small children and infants is very unique. It is rare that a company would have any interest in developing something specifically for this small and vulnerable population.”
The first patient at Seattle Children’s to receive the Renata stent was a child under the age of two who had it implanted in their pulmonary artery. Previously, the child would have received a non-pediatric stent, which would have required redilation multiple times and ultimately intentional fracture or replacement by the time they reached adolescence. But because Seattle Children’s was one of only four sites in the United States enrolled in this feasibility study, they were able to receive the Renata stent which can be expanded up to adult size and accommodate for the patient’s growth.
Q&A with Dr. Bhawna Arya
Director, Fetal Diagnosis Program and Director, Fetal Cardiology at Seattle Children’s

Can you briefly explain your roles?
As Director of the Fetal Diagnosis Program, I run the diagnostic side of the Fetal Care and Treatment Center, which provides the most comprehensive fetal care in the Pacific Northwest for babies with one or more prenatal conditions, including rare conditions that many doctors never see. In this role, I help coordinate each patient’s diagnostic next steps which, depending on the diagnosis, can mean coordinating with the neurodevelopmental team, the urology team, nephrology, surgery, palliative care, social work, genetics and many others. The priority is ensuring our patients are supported through transitions, relocations challenges and different testing as they head towards best practice therapeutics and intervention. Through this multidisciplinary approach, we optimize patient survival and safety while also ensuring the family is getting the holistic support they need.
In my other role as Director of Fetal Cardiology, I oversee the Seattle Children’s Hospital fetal cardiovascular diagnostics and coordination of care for patients from prenatal care to postnatal management. I am committed to fetal cardiovascular research locally and nationally and ensuring that we continue to make advances to improve our diagnostic capabilities and outcomes. I also support pediatric cardiologists based in Great Falls, Montana, in Anchorage and Fairbanks, Alaska, and in Yakima, the Tri-Cities, Wenatchee, Tacoma, Federal Way, Everett, Bellevue and Seattle in Washington State to make fetal cardiac diagnoses so that families do not have to travel for their evaluation. If significant fetal cardiovascular disease is identified, I work with the team to determine next steps in management.
Are you often asked for second opinions?
Yes, absolutely. We definitely get referrals from outside of the Seattle Children’s system, whether it be locally from our military colleagues or from other practices in the region, all the way to people who are looking for a second opinion from California, Colorado or further east. Even if the family ends up keeping care close to home, sometimes they just want an outside perspective to make sure that their local team is on the right track.
Why did you become a fetal cardiologist?
I'm a pediatric cardiologist by training, which means I was trained in pediatrics and then focused on cardiology for congenital heart diseases, childhood arrhythmias, other childhood cardiovascular diseases. Once that training is completed, we all shift into our own little worlds and, for me, that's taking care of moms with unborn babies with cardiovascular disease. While I enjoy the excitement of being the first one to evaluate the heart and solve the “puzzle," what’s really gratifying about this work is being able to provide the compassionate care that I think all these moms and families deserve as they’re getting perhaps some of the worst news in in their life. I connect with people in a way that feels supportive to them and allows them to grieve the loss, but then rebuild their expectations and their goals for their child's life and their families. So that's sort of the passionate side of what I do.