Publication Q&A: TGFβ Restricts Expansion, Survival and Function of T Cells Within the Tuberculous Granuloma
March 2021 – Kristin Adams, Benjamin Gern and Kevin Urdahl from Seattle Children’s Center for Global Infectious Disease Research share insights from a recent publication in Cell Host & Microbe.
TGFβ Restricts Expansion, Survival and Function of T Cells Within the Tuberculous Granuloma
Benjamin H. Gern, Kristin N. Adams, Courtney R. Plumlee, Caleb R. Stoltzfus, Laila Shehata, Albanus O. Moguche, Kathleen Busman-Sahay, Scott G. Hansen, Michael K. Axthelm, Louis J. Picker, Jacob D. Estes, Kevin B. Urdahl, Michael Y. Gerner
Published March 11, 2021
Read this article in Cell Host & Microbe.
 What are the significant findings in this paper?
What are the significant findings in this paper?
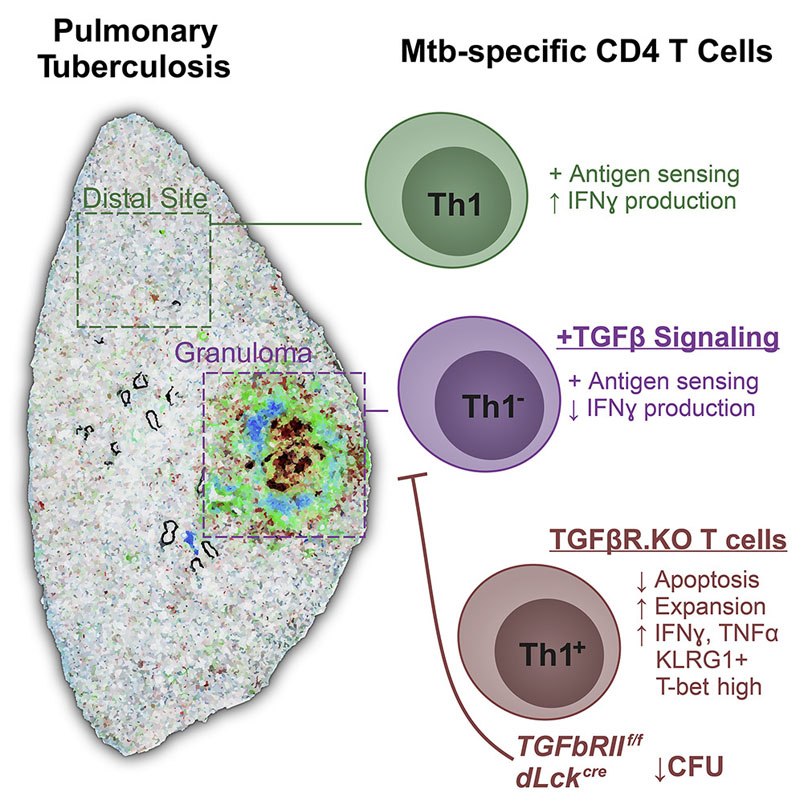
The epicenter of Mycobacterium tuberculosis (Mtb) infection is the pulmonary granuloma, an organized collection of immune and mycobacterial cells. This dynamic structure can benefit both the host (by physically containing infection) and the pathogen (by cultivating an environment that lets it persist). Understanding the factors limiting bacterial clearance within this environment is crucial for developing improved tuberculosis therapies.
Using cutting-edge microscopy, we found that immunity to tuberculosis (TB) is restricted by a factor that has recently been found to have similar effects in cancerous tumors. It does so by preventing a critically important immune cell from surviving and functioning in the granuloma environment. When we prevented this factor from acting on these cells, we improved immune responses and decreased infection. Because of the similarities between TB granulomas and tumors, this suggests that inhibitors of this factor that are currently being tested for cancer treatment may also have value to improve TB treatment.
What are the next steps and long-term goals for this research?
The next steps will be to characterize the effects of this factor on other important immune cell types within the granuloma, identify the specific cells making this factor, and understand how Mtb is promoting its production. This comprehensive approach will help inform us about which therapies might be most helpful for tuberculosis treatment. The long-term goals are to test such therapies in preclinical animal models, and ultimately identify promising candidate drugs for human clinical trials.
About the Urdahl Lab
Tuberculosis, an infectious disease caused by Mycobacterium tuberculosis (Mtb), is a global health emergency that kills nearly 1.5 million people per year, despite availability of a vaccine and antibiotic therapy. Infants and children are profoundly impacted, both because they develop more severe forms of TB than adults and because the high mortality of young adults from TB results in many single-parent households and orphans. The Urdahl Lab uses a physiologic mouse model and cutting-edge immunologic techniques to identify the barriers that prevent the immune system from mounting an effective response to Mtb infection. The ultimate goal of these efforts is to inform the design of new vaccines and therapeutics that can overcome these barriers to prevent and treat this deadly disease. Learn more about the Urdahl Lab.
Michael Gerner, PhD, from the University of Washington Department of Immunology, is also a co-corresponding author on this publication. Learn about his lab.